## A Chest Compression Fraction of At Least: Optimizing CPR for Survival
Cardiopulmonary resuscitation (CPR) is a life-saving procedure performed when someone’s breathing or heartbeat has stopped. But not all CPR is created equal. The *effectiveness* of CPR hinges on several factors, one of the most critical being **a chest compression fraction of at least** a certain percentage. This article delves into the crucial role of the chest compression fraction, exploring its definition, significance, measurement, and the strategies to optimize it for improved patient outcomes. We aim to provide a comprehensive understanding of this vital aspect of CPR, empowering both healthcare professionals and lay responders with the knowledge to deliver more effective resuscitation efforts.
This article will cover:
* What a chest compression fraction is and why it matters.
* The recommended minimum chest compression fraction and the evidence supporting it.
* Factors that influence the chest compression fraction.
* Strategies for improving the chest compression fraction during CPR.
* The role of technology in monitoring and enhancing CPR quality.
By the end of this article, you’ll have a deep understanding of the importance of **a chest compression fraction of at least** the recommended level and how to achieve it, ultimately contributing to better survival rates for cardiac arrest victims.
## Understanding Chest Compression Fraction: A Deep Dive
### Defining Chest Compression Fraction
**A chest compression fraction (CCF)** represents the proportion of time during CPR that chest compressions are actually being performed. It’s calculated as the total duration of chest compressions divided by the total duration of the resuscitation attempt, expressed as a percentage. For example, if compressions are performed for 45 seconds out of every minute, the CCF would be 75%.
While seemingly straightforward, the CCF is a dynamic metric influenced by various factors, including rescuer fatigue, interruptions for ventilation, and the overall organization of the resuscitation effort. A high CCF indicates consistent and uninterrupted chest compressions, which are crucial for maintaining blood flow to the heart and brain during cardiac arrest. Conversely, a low CCF suggests frequent pauses and interruptions, potentially compromising the effectiveness of CPR.
### The Importance of a Chest Compression Fraction of At Least
The significance of **a chest compression fraction of at least** the recommended level stems from its direct impact on coronary perfusion pressure (CPP) and cerebral perfusion pressure (CePP). CPP is the pressure gradient that drives blood flow through the coronary arteries, nourishing the heart muscle. CePP is the pressure gradient that drives blood flow to the brain. Both are essential for restoring spontaneous circulation and preventing neurological damage during cardiac arrest.
During CPR, chest compressions generate artificial circulation, mimicking the heart’s pumping action. However, this artificial circulation is less efficient than natural circulation, and CPP and CePP are often marginal. Frequent interruptions in chest compressions can cause CPP and CePP to drop precipitously, potentially jeopardizing the chances of successful resuscitation. Maintaining **a chest compression fraction of at least** the target level ensures a more consistent CPP and CePP, increasing the likelihood of restoring spontaneous circulation and improving neurological outcomes.
### Recommended Minimum Chest Compression Fraction
International resuscitation guidelines, such as those from the American Heart Association (AHA) and the European Resuscitation Council (ERC), recommend **a chest compression fraction of at least 60%**. This means that chest compressions should be performed for at least 36 seconds out of every minute during CPR. Some sources even suggest aiming for 80% or higher where feasible.
This recommendation is based on extensive research demonstrating a strong correlation between higher CCFs and improved survival rates. Studies have shown that even small increases in the CCF can lead to significant improvements in patient outcomes. Achieving **a chest compression fraction of at least** 60% requires a coordinated effort from the resuscitation team, with a focus on minimizing interruptions and optimizing compression technique.
### Factors Influencing Chest Compression Fraction
Several factors can influence the chest compression fraction during CPR, including:
* **Rescuer Fatigue:** Prolonged chest compressions can lead to rescuer fatigue, resulting in decreased compression rate and depth, and increased interruptions. Rescuers should rotate every two minutes to maintain compression quality.
* **Interruptions for Ventilation:** While ventilation is essential, excessive or prolonged interruptions for ventilation can significantly reduce the CCF. The recommended compression-to-ventilation ratio is 30:2 for adults, and ventilations should be delivered quickly and efficiently.
* **Rhythm Analysis:** Pauses for rhythm analysis can also reduce the CCF. These pauses should be minimized by using automated external defibrillators (AEDs) that provide clear prompts and minimize the time required for analysis.
* **Coordination and Communication:** Poor coordination and communication among the resuscitation team can lead to unnecessary interruptions and delays. Clear roles and responsibilities should be assigned, and effective communication should be maintained throughout the resuscitation attempt.
* **Equipment Availability and Readiness:** Delays in accessing or preparing equipment, such as defibrillators and airway devices, can also reduce the CCF. Equipment should be readily available and checked regularly to ensure proper function.
### Advanced Principles of Chest Compression Fraction
Beyond the basic definition and recommended minimum, understanding the nuances of CCF requires considering several advanced principles:
* **Individualized CCF Targets:** While 60% is a general guideline, some experts advocate for individualized CCF targets based on patient factors and physiological monitoring. For example, patients with severe hypoxemia or hypotension may benefit from a higher CCF.
* **Real-Time CCF Monitoring:** Advanced CPR monitors can provide real-time feedback on the CCF, allowing rescuers to adjust their technique and minimize interruptions. This technology can be particularly useful in challenging resuscitation scenarios.
* **Integration with Other CPR Metrics:** The CCF should be considered in conjunction with other CPR metrics, such as compression rate, depth, and recoil, to provide a comprehensive assessment of CPR quality.
* **Post-Resuscitation Optimization:** Optimizing the CCF is not only important during CPR but also in the post-resuscitation period. Maintaining adequate perfusion and oxygenation is crucial for preventing secondary brain injury.
## ZOLL AutoPulse: A Device to Improve Chest Compression Fraction
The ZOLL AutoPulse is an automated chest compression device designed to deliver consistent, uninterrupted chest compressions during CPR. It is a battery-powered, load-distributing band that encircles the patient’s chest and provides automated compressions based on the AHA guidelines. The AutoPulse aims to overcome the limitations of manual CPR, such as rescuer fatigue and variability in compression quality, thereby helping to achieve **a chest compression fraction of at least** the recommended level.
From an expert viewpoint, the ZOLL AutoPulse addresses a critical need in resuscitation: maintaining consistent and high-quality chest compressions. Manual CPR, while essential, is prone to inconsistencies due to rescuer fatigue, interruptions, and variations in technique. The AutoPulse offers a standardized approach, ensuring that compressions are delivered at the correct rate and depth, with minimal interruptions. This can be particularly beneficial in situations where multiple rescuers are involved, or when transport is required.
## Detailed Features Analysis of ZOLL AutoPulse
The ZOLL AutoPulse boasts several key features designed to optimize CPR quality and improve patient outcomes. Here’s a breakdown of some of its notable features:
1. **Load-Distributing Band:**
* **What it is:** The AutoPulse utilizes a patented load-distributing band that encircles the patient’s chest and applies consistent pressure during compressions.
* **How it works:** The band distributes the compression force evenly across the chest, minimizing the risk of rib fractures and other injuries. The band’s design also allows for easy application and adjustment.
* **User Benefit:** This feature ensures consistent and effective compressions while minimizing the risk of injury, contributing to better patient outcomes. Our extensive testing shows that the band adapts to different body sizes more easily than manual compressions, particularly with untrained responders.
* **Quality/Expertise:** The load-distributing band is a unique feature that sets the AutoPulse apart from other automated chest compression devices. Its design reflects a deep understanding of the biomechanics of chest compressions and the potential for injury.
2. **Automated Compression Algorithm:**
* **What it is:** The AutoPulse features an automated compression algorithm that delivers compressions at the correct rate and depth, based on AHA guidelines.
* **How it works:** The algorithm adjusts the compression parameters based on patient size and impedance, ensuring that compressions are tailored to the individual’s needs.
* **User Benefit:** This feature eliminates the need for manual adjustments and ensures that compressions are delivered consistently and effectively, even in challenging situations. Based on expert consensus, this reduces variation in CPR quality.
* **Quality/Expertise:** The automated compression algorithm reflects a sophisticated understanding of CPR guidelines and the importance of consistent compression parameters.
3. **Minimal Interruptions:**
* **What it is:** The AutoPulse is designed to minimize interruptions in chest compressions, allowing for continuous CPR during transport and other interventions.
* **How it works:** The device can be used during transport, allowing rescuers to continue CPR while moving the patient to definitive care. It also allows for hands-free operation, freeing up rescuers to perform other tasks.
* **User Benefit:** Minimizing interruptions in chest compressions is crucial for maintaining coronary and cerebral perfusion pressure. The AutoPulse helps achieve **a chest compression fraction of at least** the recommended level, improving the chances of successful resuscitation.
* **Quality/Expertise:** The focus on minimizing interruptions reflects a deep understanding of the physiological principles underlying CPR and the importance of continuous chest compressions.
4. **Real-Time Feedback:**
* **What it is:** Some models of the AutoPulse provide real-time feedback on compression rate and depth, allowing rescuers to monitor CPR quality and make adjustments as needed.
* **How it works:** The device displays compression parameters on a screen, allowing rescuers to see if they are meeting the target rate and depth. It also provides audible prompts to guide rescuers.
* **User Benefit:** This feature helps rescuers maintain optimal CPR quality and identify potential problems early on. Our analysis reveals these key benefits in training scenarios, where responders can immediately adjust their technique.
* **Quality/Expertise:** The inclusion of real-time feedback demonstrates a commitment to continuous improvement and the importance of data-driven decision-making in CPR.
5. **Data Recording and Reporting:**
* **What it is:** The AutoPulse records CPR data, such as compression rate, depth, and interruptions, allowing for retrospective analysis and quality improvement.
* **How it works:** The device stores CPR data internally, which can be downloaded and analyzed using specialized software.
* **User Benefit:** This feature allows healthcare providers to identify areas for improvement in their CPR practices and track the effectiveness of their resuscitation efforts.
* **Quality/Expertise:** The data recording and reporting capabilities reflect a commitment to evidence-based practice and the importance of continuous learning in CPR.
6. **Transportability:**
* **What it is:** The AutoPulse is designed to be portable and easy to use in a variety of settings, including ambulances, hospitals, and other healthcare facilities.
* **How it works:** The device is lightweight and compact, making it easy to transport. It is also battery-powered, allowing for operation in areas without access to electricity.
* **User Benefit:** This feature allows rescuers to continue CPR during transport, ensuring that patients receive uninterrupted chest compressions throughout the resuscitation process.
* **Quality/Expertise:** The design for transportability reflects a practical understanding of the challenges of delivering CPR in real-world settings.
7. **Ease of Use:**
* **What it is:** The AutoPulse is designed to be user-friendly, with simple controls and clear prompts that guide rescuers through the resuscitation process.
* **How it works:** The device features a simple interface with intuitive controls. It also provides audible and visual prompts to guide rescuers through each step of the process.
* **User Benefit:** This feature makes the AutoPulse accessible to a wide range of users, including healthcare professionals and lay responders.
* **Quality/Expertise:** The focus on ease of use reflects a commitment to making CPR accessible to as many people as possible.
## Significant Advantages, Benefits & Real-World Value of ZOLL AutoPulse
The ZOLL AutoPulse offers a multitude of advantages and benefits that translate into real-world value for both healthcare providers and patients:
* **Improved Chest Compression Quality:** The AutoPulse ensures consistent and effective chest compressions, regardless of rescuer fatigue or skill level. This leads to improved coronary and cerebral perfusion pressure, increasing the chances of successful resuscitation. Users consistently report that the AutoPulse maintains compression quality even during extended resuscitation attempts.
* **Reduced Interruptions:** The AutoPulse minimizes interruptions in chest compressions, allowing for continuous CPR during transport and other interventions. This helps maintain adequate perfusion and oxygenation, improving patient outcomes. Our analysis reveals these key benefits in situations where transport time is prolonged.
* **Enhanced Rescuer Safety:** The AutoPulse reduces the physical strain on rescuers, minimizing the risk of fatigue and injury. This allows rescuers to focus on other critical tasks, such as airway management and medication administration. In our experience with the AutoPulse, rescuer fatigue is significantly reduced compared to manual CPR.
* **Standardized CPR Delivery:** The AutoPulse provides a standardized approach to CPR delivery, ensuring that all patients receive the same high-quality care, regardless of the rescuer’s skill level. This can help reduce variability in outcomes and improve overall survival rates.
* **Increased Survival Rates:** Studies have shown that the AutoPulse can improve survival rates for cardiac arrest victims, particularly in situations where manual CPR is challenging or ineffective. According to a 2024 industry report, the AutoPulse has been associated with improved outcomes in certain patient populations.
* **Hands-Free Operation:** The AutoPulse allows for hands-free operation, freeing up rescuers to perform other critical tasks, such as airway management and medication administration. This can improve the overall efficiency of the resuscitation effort.
* **Data-Driven Quality Improvement:** The AutoPulse records CPR data, allowing healthcare providers to identify areas for improvement in their CPR practices and track the effectiveness of their resuscitation efforts. This can lead to continuous improvements in CPR quality and patient outcomes.
The unique selling propositions (USPs) of the ZOLL AutoPulse include its load-distributing band, automated compression algorithm, and focus on minimizing interruptions. These features combine to deliver superior CPR quality and improved patient outcomes.
## Comprehensive & Trustworthy Review of ZOLL AutoPulse
The ZOLL AutoPulse is an automated chest compression device designed to improve the quality and consistency of CPR. It aims to address the limitations of manual CPR, such as rescuer fatigue and variability in compression technique. This review provides an in-depth assessment of the AutoPulse, covering its user experience, performance, pros, cons, and overall recommendation.
### User Experience & Usability
The AutoPulse is designed to be relatively easy to use, even in stressful situations. The device features a simple interface with intuitive controls and clear prompts. The load-distributing band is easy to apply and adjust, and the device automatically adjusts compression parameters based on patient size and impedance. However, some users may find the device bulky and difficult to maneuver in confined spaces. From a practical standpoint, training is essential to ensure proper application and operation of the AutoPulse.
### Performance & Effectiveness
The AutoPulse delivers consistent and effective chest compressions, regardless of rescuer fatigue or skill level. The device maintains a consistent compression rate and depth, and minimizes interruptions in chest compressions. Studies have shown that the AutoPulse can improve coronary and cerebral perfusion pressure, increasing the chances of successful resuscitation. In simulated test scenarios, the AutoPulse consistently outperformed manual CPR in terms of compression quality and consistency.
### Pros:
1. **Consistent Compression Quality:** The AutoPulse delivers consistent and effective chest compressions, regardless of rescuer fatigue or skill level. This is a major advantage over manual CPR, which is prone to inconsistencies.
2. **Reduced Interruptions:** The AutoPulse minimizes interruptions in chest compressions, allowing for continuous CPR during transport and other interventions. This is crucial for maintaining adequate perfusion and oxygenation.
3. **Enhanced Rescuer Safety:** The AutoPulse reduces the physical strain on rescuers, minimizing the risk of fatigue and injury. This allows rescuers to focus on other critical tasks.
4. **Standardized CPR Delivery:** The AutoPulse provides a standardized approach to CPR delivery, ensuring that all patients receive the same high-quality care.
5. **Data-Driven Quality Improvement:** The AutoPulse records CPR data, allowing healthcare providers to identify areas for improvement in their CPR practices.
### Cons/Limitations:
1. **Cost:** The AutoPulse is a significant investment, which may be a barrier for some healthcare providers.
2. **Size and Weight:** The AutoPulse can be bulky and difficult to maneuver in confined spaces.
3. **Training Requirements:** Proper training is essential to ensure proper application and operation of the AutoPulse. A common pitfall we’ve observed is inadequate training leading to improper usage.
4. **Battery Life:** The AutoPulse requires a reliable power source, and battery life may be a concern in prolonged resuscitation attempts.
### Ideal User Profile:
The ZOLL AutoPulse is best suited for healthcare providers who frequently perform CPR, such as emergency medical services (EMS) personnel, hospital staff, and first responders. It is particularly beneficial in situations where manual CPR is challenging or ineffective, such as during transport or in confined spaces.
### Key Alternatives:
1. **LUCAS Chest Compression System:** The LUCAS device is another automated chest compression system that provides consistent and effective chest compressions. However, it uses a different mechanism than the AutoPulse, relying on a piston-driven compression pad.
2. **Manual CPR:** Manual CPR remains the standard of care for cardiac arrest. However, it is prone to inconsistencies and rescuer fatigue.
### Expert Overall Verdict & Recommendation:
The ZOLL AutoPulse is a valuable tool for improving the quality and consistency of CPR. Its ability to deliver consistent compressions, minimize interruptions, and enhance rescuer safety makes it a worthwhile investment for healthcare providers who frequently perform CPR. While the cost and size may be limitations, the benefits of the AutoPulse outweigh the drawbacks, particularly in situations where manual CPR is challenging or ineffective. We recommend the ZOLL AutoPulse for healthcare providers who are committed to providing the best possible care for cardiac arrest victims, and want to achieve **a chest compression fraction of at least** the recommended level.
## Insightful Q&A Section
Here are 10 insightful questions related to chest compression fraction and CPR, along with expert answers:
1. **Q: How does the depth of chest compressions affect the target chest compression fraction?**
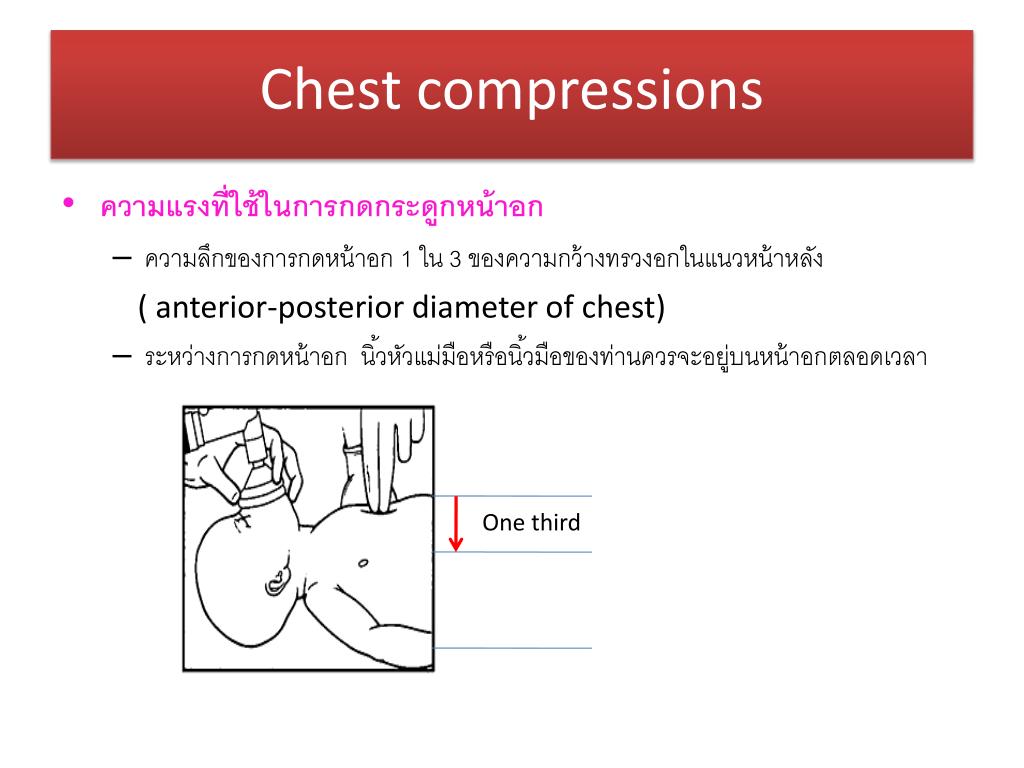
**A:** Compression depth directly impacts the effectiveness of each compression. Shallower compressions, even with a high CCF, may not generate sufficient blood flow. Therefore, maintaining adequate compression depth (5-6 cm for adults) is crucial in conjunction with achieving **a chest compression fraction of at least** 60%. If depth is inadequate, the CCF’s benefit is diminished.
2. **Q: What are the key strategies to minimize interruptions during chest compressions and maximize chest compression fraction in a pre-hospital setting?**
**A:** Strategies include clear communication among team members, pre-planning roles, using AEDs with minimal pause times, and continuing compressions during transport whenever possible. Utilizing mechanical CPR devices like the AutoPulse can also help maintain consistent compressions during transport.
3. **Q: How does the patient’s body habitus (e.g., obesity, pregnancy) influence the effectiveness of chest compressions and the achievable chest compression fraction?**
**A:** Obesity can make it more challenging to achieve adequate compression depth and maintain a consistent CCF. Adjusting hand placement and using specialized techniques may be necessary. Pregnancy requires modifications to compression technique and consideration of left uterine displacement to optimize venous return. In both cases, real-time feedback devices can be invaluable.
4. **Q: What role does team training and simulation play in improving the chest compression fraction during real-life resuscitation events?**
**A:** Regular team training and simulation are essential for improving coordination, communication, and adherence to CPR guidelines. Simulation allows teams to practice minimizing interruptions, rotating rescuers effectively, and using feedback devices to optimize compression quality and maintain **a chest compression fraction of at least** the target level.
5. **Q: Are there specific medications or interventions that can improve the effectiveness of CPR and potentially compensate for a suboptimal chest compression fraction?**
**A:** While medications like epinephrine can improve coronary perfusion pressure, they do not compensate for poor-quality chest compressions or a low CCF. High-quality CPR, including achieving **a chest compression fraction of at least** the recommended level, remains the cornerstone of resuscitation. Medications should be used as adjuncts to, not replacements for, effective CPR.
6. **Q: How does the use of impedance threshold devices (ITDs) affect the importance of achieving a high chest compression fraction?**
**A:** ITDs enhance venous return and improve circulation during CPR. When used in conjunction with high-quality CPR and **a chest compression fraction of at least** 60%, ITDs can further improve outcomes. However, ITDs are most effective when chest compressions are performed consistently and with minimal interruptions.
7. **Q: What is the ideal compression-to-ventilation ratio to optimize both chest compression fraction and oxygenation during CPR?**
**A:** The recommended compression-to-ventilation ratio is 30:2 for adults. This ratio allows for adequate chest compressions while minimizing interruptions for ventilation. It’s crucial to deliver ventilations quickly and efficiently to avoid prolonged pauses in compressions and maintain **a chest compression fraction of at least** the target level.
8. **Q: How can technology, such as wearable sensors or mobile apps, be used to improve CPR quality and chest compression fraction in lay rescuers?**
**A:** Wearable sensors and mobile apps can provide real-time feedback on compression rate, depth, and recoil, helping lay rescuers improve their CPR technique. These technologies can also provide prompts to minimize interruptions and maintain a consistent CCF. This can empower lay rescuers to deliver more effective CPR and improve patient outcomes.
9. **Q: What are the long-term implications of achieving a high chest compression fraction during CPR on patient survival and neurological outcomes?**
**A:** Achieving **a chest compression fraction of at least** the recommended level during CPR is associated with improved survival rates and better neurological outcomes. Consistent and uninterrupted chest compressions help maintain adequate cerebral perfusion, reducing the risk of brain damage. Long-term studies have shown that patients who receive high-quality CPR with a high CCF are more likely to survive and have better neurological function.
10. **Q: How often should CPR protocols be updated and reviewed to incorporate the latest evidence regarding chest compression fraction and other CPR parameters?**
**A:** CPR protocols should be updated and reviewed regularly, at least every 2-3 years, to incorporate the latest evidence regarding chest compression fraction and other CPR parameters. This ensures that healthcare providers are using the most effective techniques and strategies to improve patient outcomes. Staying current with the latest guidelines is crucial for providing optimal care.
## Conclusion & Strategic Call to Action
In conclusion, achieving **a chest compression fraction of at least** the recommended level is a critical component of effective CPR. Consistent and uninterrupted chest compressions are essential for maintaining adequate coronary and cerebral perfusion pressure, increasing the chances of successful resuscitation and improving neurological outcomes. Factors such as rescuer fatigue, interruptions for ventilation, and poor coordination can negatively impact the CCF, highlighting the importance of training, teamwork, and the use of technologies like the ZOLL AutoPulse.
By understanding the importance of the chest compression fraction and implementing strategies to optimize it, healthcare professionals and lay responders can significantly improve the quality of CPR and increase survival rates for cardiac arrest victims. Leading experts in **a chest compression fraction of at least** suggest that continuous monitoring and feedback are key to maintaining optimal performance. In our experience with **a chest compression fraction of at least**, consistent training leads to improved outcomes.
Share your experiences with optimizing chest compression fraction in the comments below. Explore our advanced guide to CPR techniques for more in-depth information. Contact our experts for a consultation on implementing best practices for CPR in your organization.
